Masks are NOT source control
Masks are NOT source control
Our intrepid PPE expert Megan Mansell explains it all.
By Megan Mansell
Particulate Range and Minimum Infective Dose
The COVID-19 conversation should have begun with minimum viable particle size under pressure, which for SARS-CoV-2-size particulates is .06 microns. This particle is under 0.3 microns, placing it firmly within the radically behaving particulate range. A single particle cluster can be composed of multiple virions and still fall well under that threshold. Furthermore, current research on aerosol behavior shows that particulates as large as 5 microns can remain aloft for extended periods. 83 COVID-19-size particles can fit in a single cluster and fall within the highest range.
The conversational pivot should have then become about respiratory emission particle size ranges: Around 90% of exhaled particulates have been shown to fall under .3 microns.
But most importantly, SARS-Cov-2 is understood to be a low-minimum-infective dose pathogen.
Minimum Infective Dose
Respiratory emissions from a transmissible individual can be shown to reach higher than 100,000 virions in one minute. We breathe an average of 16-20 times per minute, with minimum infective dose (MID) estimated by current research to be 100-1000 virions ( 1, 2, 3, 4), where the most conservative calculations of MID based on these findings show that one exhale can have enough viral load to infect 5 or more people in an enclosed space.
Comparison studies of different respiratory viruses and SARS-CoV-2 animal studies have been used to contribute to current MID estimates.
The mechanics of exacerbation due to focused plumes of fine particulates and aerosolization of droplets
Exhale matters a great deal with an airborne pathogen. Every breath increases the atmospheric viral load (the amount of viral matter held aloft) in an enclosed space. When it doesn’t take very much of an airborne pathogen for vulnerable individuals to get sick, a contagious individual should not wear a mask or respirator that creates a concentrated plume of aerosols, thinking they are protecting others.
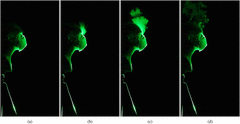
Plosive force generating events, such as coughs and sneezes, increase the pressure behind exhale emissions. Masks can exacerbate the spread of airborne pathogens due to focused plumes of fine particulates that increase the emission trajectory and aerosolization of droplets through a membrane. Aerosols have a trajectory of 18-20 feet, but pressure behind droplets through a membrane can take this larger matter that would have fallen in a predictable 6-ish foot arc and turn it into aerosols, as well as nebulize bound particulates on inhale.
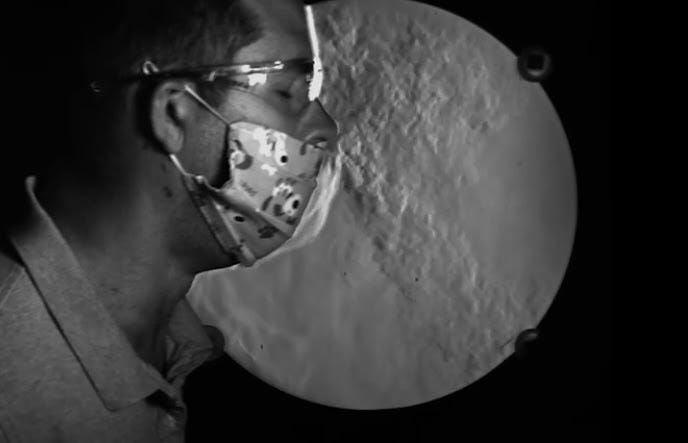
Exhaled emissions take the path of least resistance, either through the mask,
or out the sides, as seen in this viral video of many different kinds of masks (image still from video)
Consider, for instance, the ramifications of the path of least resistance when the plume from one of the people below is directed straight at the face of the person next to him.
All masks and respirators are not created equal and are not interchangeable.
Cloth and Surgical Masks
Cloth masks have been shown to have 97% particle penetration, with 44% for surgical masks.
Tyndall lighting used in emissions imaging is capable of showing smaller particle size ranges of aerosols (.04-0.9 microns), but not all imaging uses this, and most studies are not clear about their lighting sources. Most of what you see in an emitted plume begins at the 50 micron+ range – so what is clearly demonstrated by plume emission imaging is that masks are incapable of stopping even the “big guys” (droplet range pathogens) from escaping.
Note the outward respiratory-range trajectory of emitted particulates. Cloth masks are expressly non-PPE, non-mitigating apparatuses per OSHA and NIOSH standards for airborne pathogens due to this reason – their fit and matrix composition are not sufficient for radically behaving particulate range pathogens.
“But surgeons use surgical masks…”
Postoperative wound infection rates are not improved by surgical masking. Surgeons wear them to prevent splatters and sprays of bodily fluids from reaching oral and nasal mucosa, not to protect themselves or others from airborne pathogens, for which they are expressly non-mitigating per OSHA and NIOSH standards.
Respirators
Some higher-grade respirators do meet minimum particle filtration standards for personal protection, but even these apparatuses do not filter COVID-19-size particulates on exhale.
Why does this matter? We heard “DROPLET” nonstop for 6 months before any governing body began acknowledging airborne spread, without ever correcting course on our nation’s PPE recommendation considerations, especiallyas source control.
For instance, this is a test site photo of the person most likely to be in contact with novel pathogens.
The exhale plume of emissions created by this mask is directly over the testing materials (oftentimes run with PCR thresholds too high to indicate live viral matter) and is breathed directly into car windows. Mistakes were made, yet masks were still forced on our global populace, many of whom were punished for noncompliance, while 71% of new cases report always masking, and 14% report masking most of the time, per the CDC.
Masks are *clearly* not source control, even with unvented N95s, which are the baseline minimum as a personal protective measure, and even so do not show high efficacy rates in real-world application.
Other creative yet non-mitigating methods implemented during the pandemic include, but are not limited to:
Face shields
And the method for those who forgot hankies exist:
Biological Amplification
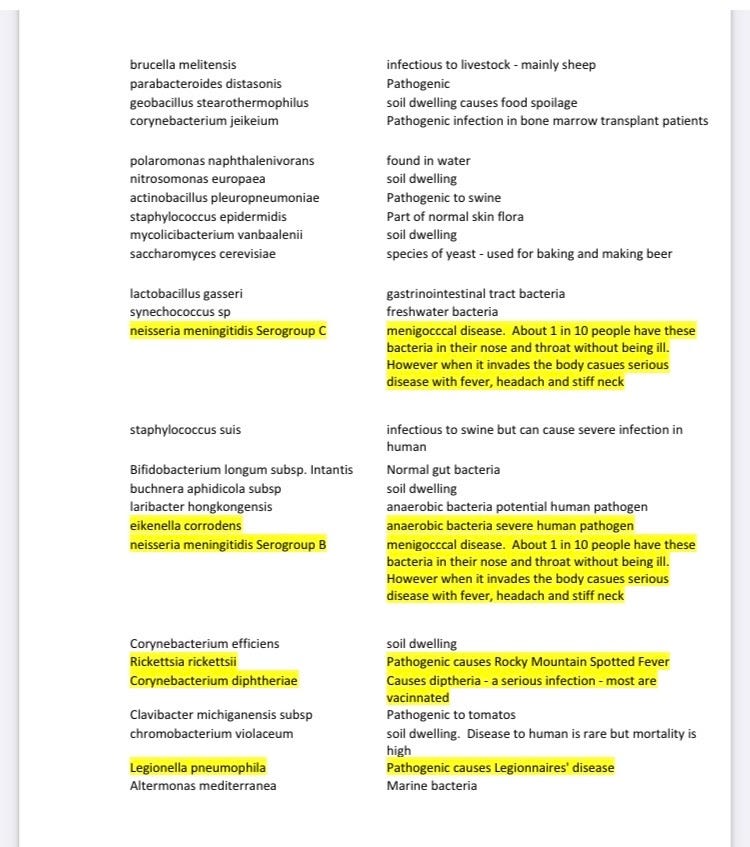
Not only is there an accumulation of rejected respiratory emissions in mask dead space, but also biological amplification of rejected bodily waste picked up from inhaled airborne microbes, in addition to periodontal bacterial contributions, which thrive in low-oxygen, warm, moist areas.
Masks come with grave microbial inhalation issues (as many adults and children wear them in public restrooms [toilet plumes 🤢], drop them, sneeze in them, run in them, and put them right back on their faces to breathe the accumulation of rejected matter for 8-12 hours per day).
Medical consent belongs in all conversations involving non-standard public integration requirements, most especially those shown to be dangerous from multiple angles for a 99.8% survivability-rate pathogen.
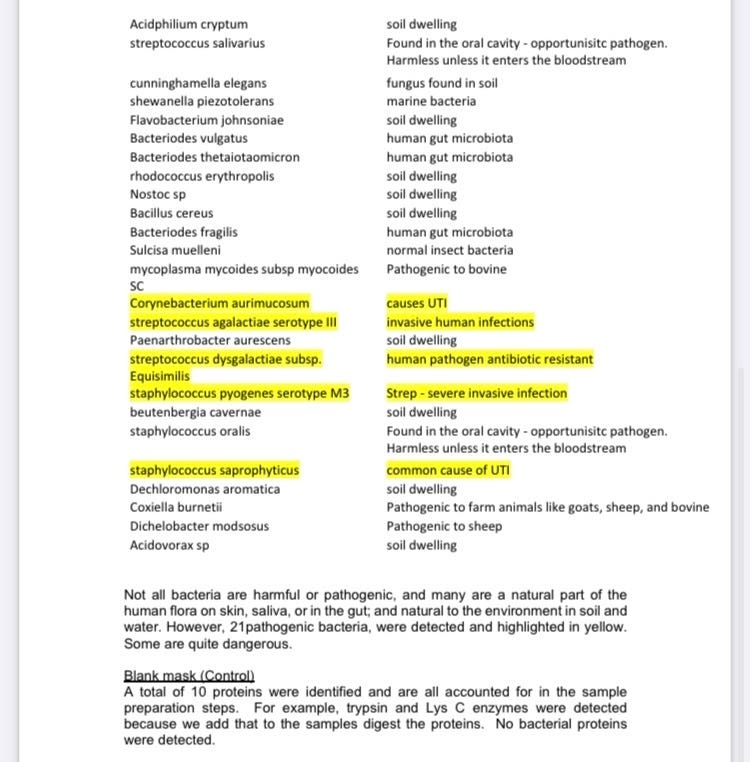
These are the microbial findings on a mask sampled after one day of wear (and freshly washed before wearing):
We are engaging in dangerous practices by requiring apparatuses that are shown to be harmful from so many angles. For the protection of people of all ages, we must encourage a national pivot to focused protective measures for our vulnerable populations, including the implementation of the hierarchy of controls, and step away from dependency on mismatched apparatuses that have taken us down this road to hell paved with good intentions.
Being incredibly specific about the predictable behavior of particulates is critical when trying to create national standards to follow for current and future outbreaks.
Megan Mansell is a former district education director over special populations integration, serving students who are profoundly disabled, immunocompromised, undocumented, autistic, and behaviorally challenged; she also has a background in hazardous environs PPE applications. She is experienced in writing and monitoring protocol implementation for immunocompromised public sector access under full ADA/OSHA/IDEA compliance. She can be reached at MeganKristenMansell@Gmail.com.






Comments
Post a Comment