A Fantasy of Virus-Free Air
A Fantasy of Virus-Free Air
Are periodic respiratory virus infections necessary to maintain overall human health?
More than twenty months into the pandemic, it’s clear that many mandated mitigation strategies do not significantly prevent virus transmission, or do so at a steep price. Lockdowns haven’t stopped virus spread around the world, and are not sustainable due to massive collateral damage. There is no consistent evidence of a benefit of universal masking, despite unprecedented politicization and potential for bias in scientific studies. School closures and remote learning are harmful and ineffective, as children remain at low risk for severe disease and schools are not major drivers of community outbreaks. Vaccines may limit severe disease, which is important for vulnerable individuals, but are less effective at preventing infection and transmission than immunity acquired by infection. Despite a lack of compelling evidence, many leaders continue mandating unproven and unnecessary restrictions on a COVID-fatigued population.
However, amidst these failures, one effective COVID-19 mitigation strategy stands out—improving indoor ventilation. It was known quite early in the pandemic that outdoor transmission of SARS-CoV-2 was rare, and that indoor transmission was frequently associated with crowded and poorly ventilated spaces (although this did not stopped leaders from cancelling outdoor events and mandating outdoor restrictions). Strategies to increasing ventilation have survived 20 months of failed efforts because strong evidence supports their continued development and utility.
Ventilation: The NPI That Works for Airborne Viruses
In commercial aircraft—one example of a highly ventilated indoor space—virus transmission has been low despite crowded conditions. This has been attributed to forced masking of passengers (unfortunately including children with disabilities). However, pressurized aircraft cabins experience 20-30 air changes per hour (ACH), meaning all of the air within a cabin will be filtered and replaced every 2-3 minutes. With this level of ventilation, the ability of a person to expose an individual to an infectious dose even in the next seat is quite limited. A classic example of a commercial aircraft outbreak was in 1977, where a single passenger with influenza infected 72 percent of other passengers on the flight. This extraordinary event required a complete failure of the ventilation system and a three-hour delay on the tarmac. If the ventilation system had been functional, the outbreak would have never happened.
To give an idea of how ventilation increases the time to infectious dose compared to cloth (typical) masking, below is a table created using model calculations created by Dr. Lisa Brosseau, an expert with over 30 years of experience in PPE and particle filtration:
Although this table was created to illustrate the potential for high-quality respirators to decrease time to infectious dose (for workers in high-risk situations), you can also see the advantages of increased ventilation. As ACH increases, the time to infectious dose increases much more significantly than with face coverings, with differences that can be measured in hours for ventilation compared to minutes for masking.
Increasing indoor ventilation is an effective strategy because airborne transmission is a significant route for SARS-CoV-2 spread, while surface transmission is not. Airborne virus may remain suspended in small aerosol particles for hours, rendering typical face coverings ineffective (and extended use of N95-type respirators is simply not practical). The 6-foot rule for social distancing, based early estimates of surface of large droplets, also becomes increasingly arbitrary in an airborne transmission scenario. These facts make adjustments to indoor ventilation an attractive strategy for building engineers seeking to decrease the risk of airborne virus transmission.
There are many buildings where this strategy could make a big difference, such as assisted living facilities. Hospitals already incorporate these strategies to significant effect. Anywhere where vulnerable individuals congregate in significant numbers might consider ventilation strategies designed to minimize transmission of respiratory viruses.
A Sterile Air Pipe Dream
But, as with any mitigation strategy, what can be done can also be overdone (this might be an unofficial motto of the U.S. pandemic response). In September, the Atlantic published an article titled “The Plan to Stop Every Respiratory Virus at Once”:
The article begins by outlining the historical advances in sanitation and purification of drinking water in ending cholera outbreaks and measures targeting mosquitos and mosquito-breeding habitats that minimized threats from yellow fever and malaria. The author then compares these efforts to a lack of concern for building ventilation, an issue highlighted by the COVID-19 pandemic and high levels of transmission in crowded and poorly ventilated spaces, and applies the same logic: “We don’t drink contaminated water. Why do we tolerate breathing contaminated air?”
“It’s not just about COVID-19. The scientists who recognized the threat of airborne coronavirus early did so because they spent years studying evidence that—contrary to conventional wisdom—common respiratory illnesses such as the flu and colds can also spread through the air. We’ve long accepted colds and flus as inevitable facts of life, but are they? Why not redesign the airflow in our buildings to prevent them, too?”
Building engineers believe that measures used during the current pandemic aren’t enough: “The pandemic has already prompted, in some schools and workplaces, ad hoc fixes for indoor air: portable HEPA filters, disinfecting UV lights, and even just open windows.” But in their eyes, these aren’t long-term solutions. “Modern buildings have sophisticated ventilation systems to keep their temperatures comfortable and their smells pleasant—why not use these systems to keep indoor air free of viruses too?”
To her credit, the author issues this caveat: “No one I spoke with thought an average school or office building has to be as tightly controlled as a biocontainment facility, but if not, then we need a new and different set of minimum standards.” She also rightly compares relative threat levels of intestinal pathogens—that she used earlier as analogous—and COVID-19: “COVID-19 does not kill as high a proportion of its victims as cholera did in the 19th century. But it has claimed well over 600,000 lives in the U.S. Even a typical flu season kills 12,000 to 61,000 people every year. Are these emergencies? If so, what would it take for us, collectively, to treat them as such?”
There are some obvious barriers to engineering every building with virus-scrubbing ventilation: “The pandemic has made clear that Americans do not agree on how far they are willing to go to suppress the coronavirus. If we can’t get people to accept vaccines and wear masks in a pandemic, how do we get the money and the will to rehaul all our ventilation systems?” Thus, the real problems are the usual suspects—money and the unwillingness of others to take the problem seriously. But, as many a strategy has been rationalized in the last two years, if it can save lives, why not do it? “The changes might take too long to matter for this current pandemic, but there are other viruses that spread through the air, and there will be more pandemics.”
I believe—in agreement with building engineers and indoor environmental scientists—that it’s possible to design ventilation systems with the ability to scrub the air of all airborne respiratory viruses. I also agree that this might have a measurable benefit in one aspect of human health, as the disease burden of respiratory viruses is significant.
Yet, as Martin Kulldorff and others have tried to remind the world, public health isn’t just about preventing one infectious disease at all costs, and there’s a potential cost to virus-free air that has not been considered: What if periodic infections by respiratory viruses are necessary to maintain overall human health? Did the miracles of clean water and improved sanitation have only obvious benefits, with no costs?
The Example of Polio
In addition to influenza and smallpox, polio was also considered a major viral pathogen of the 20th century. However, before that time, it wasn’t thought to be a major threat. There weren’t serious outbreaks. It wasn’t as if the virus didn’t exist. People had been infected with polio for thousands of years. But with the advent of the industrial revolution, our relationship with the virus changed, and so did the disease it caused.
Polio is a highly contagious virus that causes an asymptomatic (yet still transmissible) or very mild symptomatic infection in 90% of people. The virus infects the gastrointestinal tract of humans, although in some cases, the virus spreads to the nervous system, and can result in paralysis or death. Because so many people are asymptomatic, the virus can infect many others before a paralytic case is identified, making it difficult to contain. The virus is transmitted by the fecal-oral route, through water and other fecal contaminated material.
For most of human history, people could not avoid being infected with polio virus. Most were infected during infancy. And since almost everyone was infected, they had antibodies, including new mothers who were passing those antibodies on to their children through the placenta prior to birth and via breastfeeding afterwards. Infantile paralysis, although still possible, was relatively rare.
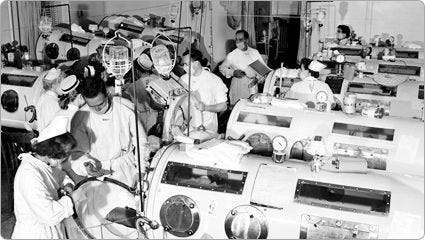
But then sanitation improved. Indoor plumbing, water and sewage treatment became more widely adopted. Families began to live in cleaner, less crowded conditions. People were no longer exposed to polio as infants. And when older children and young adults got polio, nerve destruction and paralysis became more frequent. Some cases were so severe, that individuals suffered paralysis of the diaphragm and intercostal muscles, which are essential for breathing. They had to be administered artificial respiration with a Drinker respirator, also known as the Iron Lung, until they recovered. If they recovered. Others lived with partial paralysis for the rest of their lives.
The polio virus was no longer an endemic virus, and had ceased to coexist with humans the way it had evolved for thousands of years. And where it lost its endemic status, it gained epidemic potential. And these epidemics just so happened to hit wealthy people, since clean conditions were a sign of wealth, and thus the rich were less likely to have immunity to polio from infancy.
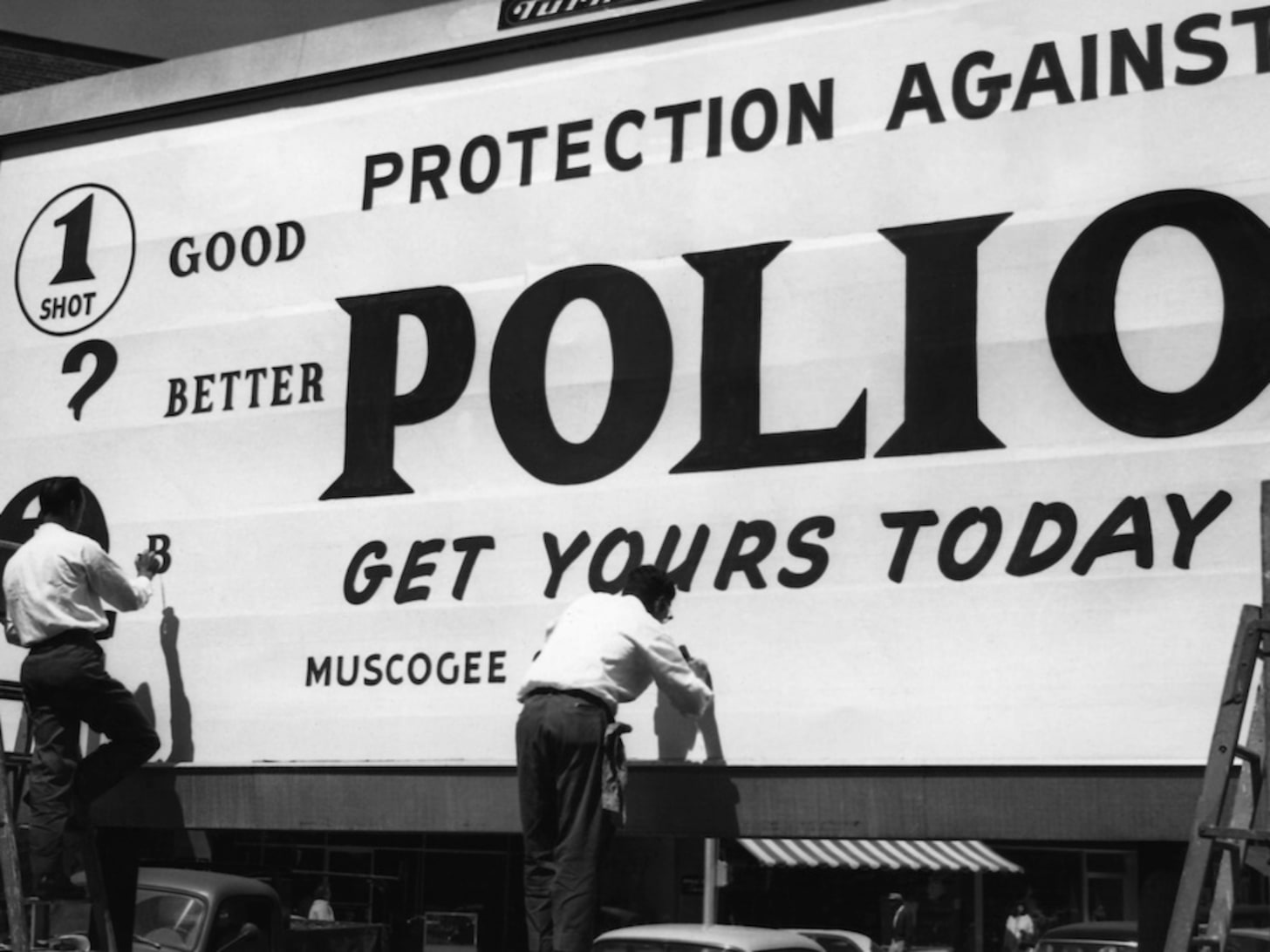
Because it was impossible to predict where and who polio could strike, strict measures were taken to avoid polio exposure. Swimming pools and beaches were closed for the summer in the early 1950s, at the height of the worst polio epidemic in the United States. Children had to stay away from crowds and were often banned from public places. There were crazy rumors that soft drinks or changes in temperature or weather were spreading the disease. People refused to shake hands. Yet people didn’t need to hear horror stories in order to manipulate their behavior, they were eyewitnesses, and seeing their neighbor lose a child to polio was all the evidence that was needed to encourage cautious behavior.
As with smallpox, the only thing that ended the polio outbreaks was a return to population immunity - mitigation measures were much less effective, and only delayed inevitable outbreaks. As with smallpox, population immunity was increased through mass vaccination. Since polio vaccines confer long-lived immunity, polio is no longer a problem in developed countries, although, unlike smallpox, it has yet to be eradicated.
A Consequence of Sanitized Indoor Air: Increased Immune Ignorance
The subsequent rise of polio epidemics with improved sanitation suggests that just because an advance in public health has immediate and obvious benefits, doesn’t mean there won’t be a cost that isn’t immediate or obvious.
This is also true of indoor environments—the “cleaner” the indoor environment that children are exposed, the more likely they are to develop chronic inflammatory diseases later in life. This has been demonstrated in a number of studies comparing geographically and genetically similar populations with different home environments. Children reared in environments that expose them to a variety of bacteria appear to have immune systems that are “educated” to tolerate those bacteria and other biological microparticles, while those in “clean” environments have immune systems that could be described as “ignorant” and thus more likely to overreact.
It is possible that respiratory viral infections also have some developmental benefit, but this field is in its infancy. Every living thing has co-evolved with viruses (humans are often infected with viruses without being aware of them), and thus it’s not a stretch to believe that preventing all respiratory viral infections might also have a latent cost.
One potential cost is a loss of immune memory to respiratory viruses. Not only would living in virus-free air result in decreased specific antiviral immunity, it would also eliminate heterologous or cross-immunity. Heterologous immunity is defined as the induction of an immune response to an unrelated pathogen/antigen upon exposure to a different pathogen/antigen.
Many working parents have experience with heterologous immunity, and sometimes a lack of it, often with out realizing it. When a firstborn child goes into daycare, weeks to months old, all microbial hell breaks loose (or at least it seems like it). The baby is sick all of the time, and so are the parents. This can go on for months, and is especially bad during the cold and flu season.
However, the next year, it gets better. And with a second child, everyone doesn’t get as sick, and that’s not just a figment of the parents’ imagination. That’s because immune memory has been acquired by the parents and the older sibling that protects against the same cold and flu viruses, and also offers a degree of cross-protection against other viruses with similar properties. The second baby doesn’t get as sick either, as he/she gets some protection from mother’s antibodies and less infections from their own immune-strengthened family.
The pandemic has introduced the concept of heterologous immunity to many non-immunologists. Lymphocytes isolated from individuals prior to the pandemic were still found to be cross-reactive to parts of SARS-CoV-2 proteins. Although the microbes that originally activated these cross-reactive cells haven’t been identified, they might be other circulating coronaviruses. Heterologous immunity also likely protected some people during the 1918 Spanish flu pandemic—those that were protected after recovery from an earlier, less lethal strain, and older people that may have been protected by long-lasting immunity from previous flu epidemics.
This raises some important questions about the downsides of a complete overhaul of current building design to eliminate common respiratory virus infections. Even if widespread adoption of these plans was feasible, would the potential loss of cross-immunity in healthy individuals be worth it? Much like non-pharmaceutical interventions have only delayed viral spread in the current pandemic (if they’ve had any effect), wouldn’t these measures just delay the inevitable? Even if many buildings have clean, virus-free air, there will always be places that don’t, mainly in older buildings concentrated in older areas with higher poverty rates. Like with polio, this could actually increase epidemics among the wealthy once certain respiratory viruses evolve ways to overcome modern building engineering.
Novel vaccines could contribute to immunity and cross-immunity, as with polio, yet these have been less effective for respiratory viruses. And as the author of the Atlantic article mentioned, we can’t agree on masks and vaccines, even during a pandemic. It’s unlikely many people would be willing to be vaccinated against every cold and flu virus for normal seasonal spread if they are healthy and low-risk. And why would they? Same for building designers engineering all new buildings to be virus-free as well as energy efficient. In this case, the will to act may not be necessary, even without consideration of potential downsides.
In our current safety culture-driven pandemic response, any risk of infection is deemed unacceptable, and those who highlight potential costs of mitigation measures are labeled irresponsible and dangerous. However, safety worship and building engineers might override old-fashioned common sense, but they can’t override our own biology. The old adage survives despite our best efforts; in the case of seasonal cold and flu viruses, what doesn’t kill you still makes you stronger.


Comments
Post a Comment